
Health
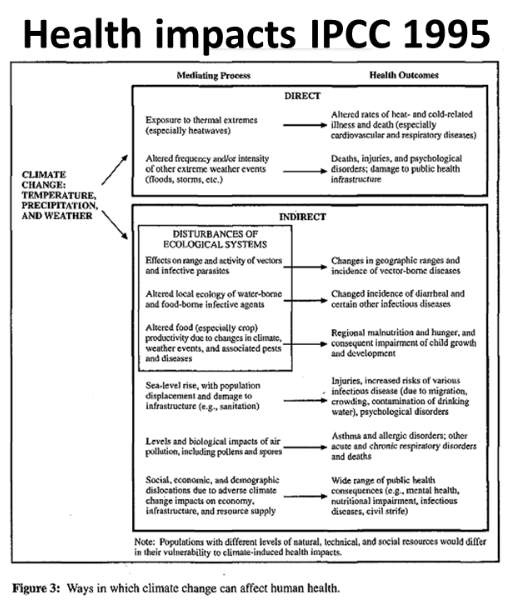
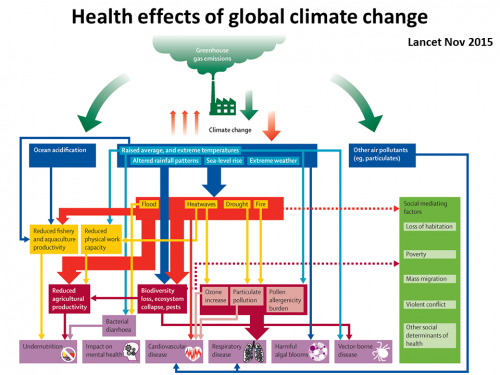
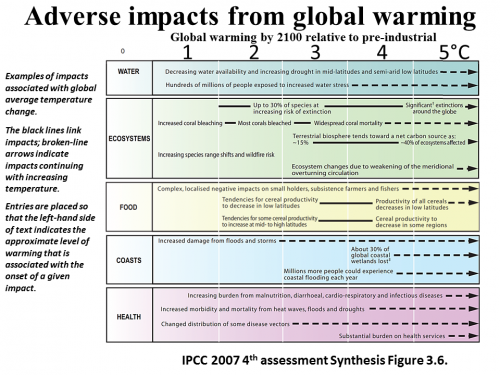
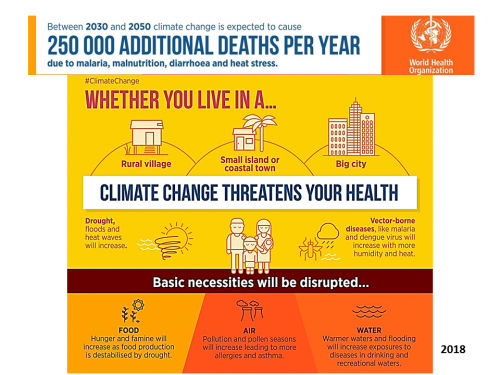
The health effects of global warming and climate change have been well known for decades. as the 1995 IPCC chart shows.
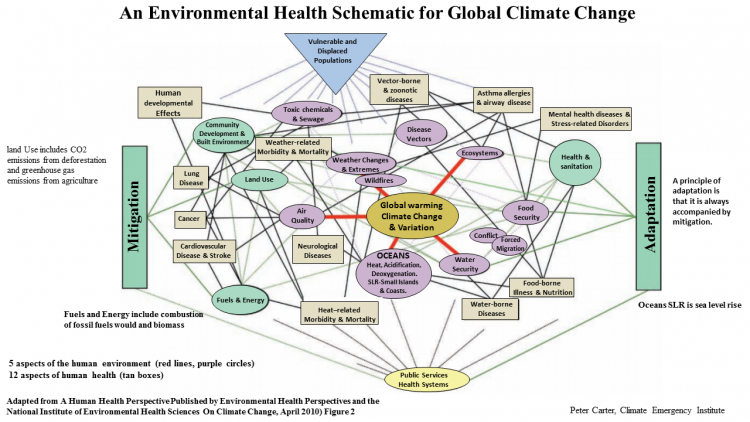
The actual problem is atmospheric GHG pollution with severe environmental health impacts and risks impacts. How ever this is not how the issue is being addressed.
The populations in Africa and lower latitude regions have always been recognized as most vulnerable to all these impacts, and it has been assumed that the wealthy industrially developed nations would be able to cope with the less severe impacts affecting their populations.
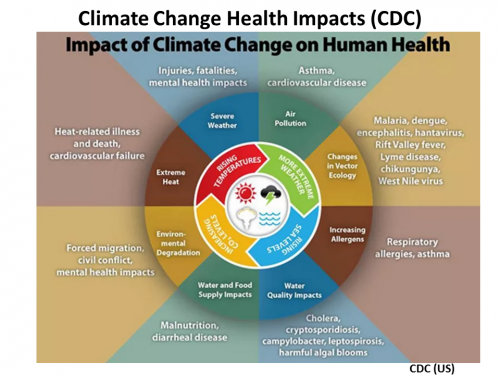
Extreme weather events that are already increasing from global climate change, are the most damaging to human life and health.
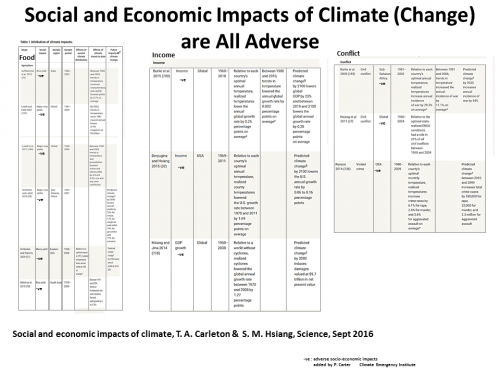
The most climate vulnerable regions are already suffering negative effects on crop yields (IPCC 2014 AR5).
With records to water security climate change is increasing both droughts and floods, and large lakes are drying up- e.g 2016 Bolivia's second largest lake).
Forty per cent of the worlds population rely on the spring melt of Himalaya glaciers for their water supplies. 2012 research found that these glaciers are melting away faster than had been thought.
2016 research found that Climate change deteriorates water quality in the Himalayas affecting 40 percent of world's population
The actual problem is atmospheric GHG pollution with severe environmental health impacts and risks impacts. How ever this is not how the issue is being addressed.
The populations in Africa and lower latitude regions have always been recognized as most vulnerable to all these impacts, and it has been assumed that the wealthy industrially developed nations would be able to cope with the less severe impacts affecting their populations.
Extreme weather events that are already increasing from global climate change, are the most damaging to human life and health.
The most climate vulnerable regions are already suffering negative effects on crop yields (IPCC 2014 AR5).
With records to water security climate change is increasing both droughts and floods, and large lakes are drying up- e.g 2016 Bolivia's second largest lake).
Forty per cent of the worlds population rely on the spring melt of Himalaya glaciers for their water supplies. 2012 research found that these glaciers are melting away faster than had been thought.
2016 research found that Climate change deteriorates water quality in the Himalayas affecting 40 percent of world's population
CLIMATE SYSTEM EMERGENCY INSTITUTE
The UK-based Climate and Health Council
2012 IPCC Special Report Risks of Extreme weather disasters
Small children are most vulnerable to the climate change health impacts. 2017 paper Pollution from Fossil-Fuel Combustion is the Leading Environmental Threat to Global Pediatric Health
Feb 2018 WHO Climate Change and Health
June 2015 Climate change health risk is a "medical emergency", experts warn- University College London's (UCL) Institute for Global Health.
Feb 2018 WHO Climate Change and Health
June 2015 Climate change health risk is a "medical emergency", experts warn- University College London's (UCL) Institute for Global Health.
IPCC AR5 2014 Health Chapter
Exec Summary The health of human populations is sensitive to shifts in weather patterns and other aspects of climate change (very high confidence). These effects occur directly, due to changes in temperature and precipitation and occurrence of heat waves, floods, droughts, and fires. Indirectly, health may be damaged by ecological disruptions brought on by climate change (crop failures, shifting patterns of disease vectors), or social responses to climate change (such as displacement of populations following prolonged drought). Variability in temperatures is a risk factor in its own right, over and above the influence of average temperatures on heat-related deaths. Biological and social adaptation is more difficult in a highly variable climate than one that is more stable.
Until mid-century climate change will act mainly by exacerbating health problems that already exist (very high confidence). New conditions may emerge under climate change, and existing diseases (e.g., food-borne infections) may extend their range into areas that are presently unaffected (high confidence). But the largest risks will apply in populations that are currently most affected by climate related
diseases.
Thus, for example, it is expected that health losses due to climate change-induced undernutrition will occur mainly in areas that are already food-insecure. In recent decades, climate change has contributed to levels of ill health though the present worldwide burden of ill health from climate change is relatively small compared with other stressors on health and is not well quantified. Rising temperatures have increased the risk of heat-related death and illness. Local changes in temperature and rainfall have altered distribution of some water-borne illnesses and disease vectors, and reduced food production for vulnerable populations.
If climate change continues as projected across the Representative Concentration Pathway (RCP) scenarios, the major changes in ill health
compared to no climate change will occur through:
• Greater risk of injury, disease, and death due to more intense heat waves and fires (very high confidence)
• Increased risk of undernutrition resulting from diminished food production in poor regions (high confidence)
• Consequences for health of lost work capacity and reduced labor productivity in vulnerable populations (high confidence)
• Increased risks of food- and water-borne diseases (very high confidence) and vector-borne diseases.
In addition to their implications for climate change, essentially all the important climate-altering pollutants (CAPs) other than carbon dioxide (CO2) have near-term health implications (very high confidence). In 2010, more than 7% of the global burden of disease was due to inhalation of these air pollutants (high confidence).
The capacity of the human body to thermoregulate may be exceeded on a regular basis, particularly during manual labor, in parts of the world during this century.
In the highest Representative Concentration Pathway, RCP8.5, (business as usual) by 2100 some of the world’s land area will be experiencing 4°C to 7°C higher temperatures due to anthropogenic climate change If this occurs, the combination of high temperatures and high humidity will compromise normal human activities, including growing food or working outdoors in some areas for
parts of the year.
The most effective measures to reduce vulnerability in the near term are programs that implement and improve basic public health measures such as provision of clean water and sanitation, secure essential health care including vaccination and child
health services, increase capacity for disaster preparedness and response, and alleviate poverty (very high confidence).
Exec Summary The health of human populations is sensitive to shifts in weather patterns and other aspects of climate change (very high confidence). These effects occur directly, due to changes in temperature and precipitation and occurrence of heat waves, floods, droughts, and fires. Indirectly, health may be damaged by ecological disruptions brought on by climate change (crop failures, shifting patterns of disease vectors), or social responses to climate change (such as displacement of populations following prolonged drought). Variability in temperatures is a risk factor in its own right, over and above the influence of average temperatures on heat-related deaths. Biological and social adaptation is more difficult in a highly variable climate than one that is more stable.
Until mid-century climate change will act mainly by exacerbating health problems that already exist (very high confidence). New conditions may emerge under climate change, and existing diseases (e.g., food-borne infections) may extend their range into areas that are presently unaffected (high confidence). But the largest risks will apply in populations that are currently most affected by climate related
diseases.
Thus, for example, it is expected that health losses due to climate change-induced undernutrition will occur mainly in areas that are already food-insecure. In recent decades, climate change has contributed to levels of ill health though the present worldwide burden of ill health from climate change is relatively small compared with other stressors on health and is not well quantified. Rising temperatures have increased the risk of heat-related death and illness. Local changes in temperature and rainfall have altered distribution of some water-borne illnesses and disease vectors, and reduced food production for vulnerable populations.
If climate change continues as projected across the Representative Concentration Pathway (RCP) scenarios, the major changes in ill health
compared to no climate change will occur through:
• Greater risk of injury, disease, and death due to more intense heat waves and fires (very high confidence)
• Increased risk of undernutrition resulting from diminished food production in poor regions (high confidence)
• Consequences for health of lost work capacity and reduced labor productivity in vulnerable populations (high confidence)
• Increased risks of food- and water-borne diseases (very high confidence) and vector-borne diseases.
In addition to their implications for climate change, essentially all the important climate-altering pollutants (CAPs) other than carbon dioxide (CO2) have near-term health implications (very high confidence). In 2010, more than 7% of the global burden of disease was due to inhalation of these air pollutants (high confidence).
The capacity of the human body to thermoregulate may be exceeded on a regular basis, particularly during manual labor, in parts of the world during this century.
In the highest Representative Concentration Pathway, RCP8.5, (business as usual) by 2100 some of the world’s land area will be experiencing 4°C to 7°C higher temperatures due to anthropogenic climate change If this occurs, the combination of high temperatures and high humidity will compromise normal human activities, including growing food or working outdoors in some areas for
parts of the year.
The most effective measures to reduce vulnerability in the near term are programs that implement and improve basic public health measures such as provision of clean water and sanitation, secure essential health care including vaccination and child
health services, increase capacity for disaster preparedness and response, and alleviate poverty (very high confidence).
Extreme weather events increased by global climatge change are the most damaging of impact ctaegories to human health and the crops.
However in general the IPCC assessments treat human health as seperate from extreme weather, and these impacts are not assessed in combination.
However in general the IPCC assessments treat human health as seperate from extreme weather, and these impacts are not assessed in combination.
Environmental health risk assessment of total pollution health impacts by SOURCES Climate change should be assessed by an environmental health risk assessment, not only by a climate change assessment. The IPCC refers to risk but does not in fact apply risk to the assessments.
Industrial energy pollution
As is well known Fossil fuel energy production causes deadly health impacts from air pollution as well as from climate change. While deaths from global climate change are estimated in the hundreds of thousands, deaths from fossil fuel air pollution are estimated to be three million a year (IEA 2016).
Global climate change increases air pollution, so as global climate change increases so will the millions of deaths. Gasoline combustion by vehicle exhausts increases the risk of cancers, particularly affecting children. Coal in particular increases the risk of cancers and also emits mercury which is a neurological toxin.
Fossil fuel air pollution is a cause that increases the risk of respiratory disease, cardiovascular disease, cancers, neurological disease, diabetes, and adverse outcomes of pregnancy.
Industrial age food production pollution
A large source of methane emissions is the livestock meat industry. Methane is exhaled by ruminant digestion. Meat is also a large the cause of human disease. Meat increases the risk of cardiovascular disease, colorectal cancer and type 2 diabetes.
Industrial energy pollution
As is well known Fossil fuel energy production causes deadly health impacts from air pollution as well as from climate change. While deaths from global climate change are estimated in the hundreds of thousands, deaths from fossil fuel air pollution are estimated to be three million a year (IEA 2016).
Global climate change increases air pollution, so as global climate change increases so will the millions of deaths. Gasoline combustion by vehicle exhausts increases the risk of cancers, particularly affecting children. Coal in particular increases the risk of cancers and also emits mercury which is a neurological toxin.
Fossil fuel air pollution is a cause that increases the risk of respiratory disease, cardiovascular disease, cancers, neurological disease, diabetes, and adverse outcomes of pregnancy.
Industrial age food production pollution
A large source of methane emissions is the livestock meat industry. Methane is exhaled by ruminant digestion. Meat is also a large the cause of human disease. Meat increases the risk of cardiovascular disease, colorectal cancer and type 2 diabetes.
My Paper Climate Impacts Responses 2016 Environmental Health Risk Assessment to Correct Climate Change Policy-making Failure, International Conference on Climate Change:Impacts & Responses.
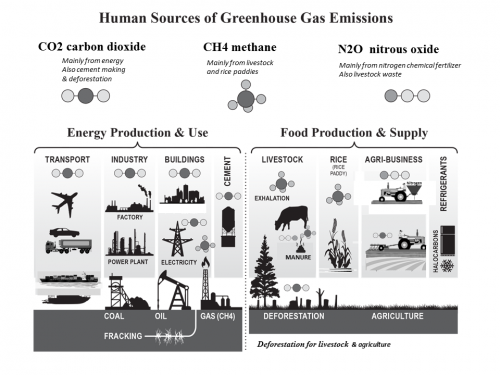
Greenhouse gas emissions can be conveniently be broadly divided into two large sources. The main one is carbon combustion for energy. The other, not far behind it when including deforestation for the livestock to meat industry, is food production. Increasingly the research is showing that the two big factors in the chronic degenerative diseases of the industrially developed world are fossil fuel air pollution and are less than healthy diets.
The impacts of global climate change on human health comes under the discipline of environmental health risk assessment and management. This differs from the IPCC and other climate change assessments in that the pollutants from the sources of the greenhouse gas emissions are included along with the greenhouse gas emissions. From the environmental health perspective by far the greatest damaging human health impact is from fossil fuel air pollution, which the research says will be increased by global warming and climate change.
The two main sources of air pollution's damaging effects on human health are ground level surface ozone and particulate matter. Surface ozone is produced as a chemical reaction from fossil fuel air pollutants catalyzed by solar warmth. Therefore surface ozone increases with global warming. It is highly irritant to the respiratory tract. The research is showing that surface warming and air circulation effects will increase the adverse effects from particulate matter.
“Ground level ozone is formed through photochemical reactions that involve nitrogen oxides (NOx), carbon monoxide (CO), methane (CH4), and volatile organic compounds (VOCs) in the presence of sunlight and elevated temperatures. Therefore as temperatures rise, many air pollution models project increased ozone production, especially within and surrounding urban areas. It is highly irritant to the entire respiratory tract. "There is observed evidence that tropospheric ozone increases in extreme heat, resulting in air pollution mortality” (IPCC 2014, 728-729).
There is evidence that global warming and climate change will increase the adverse impacts of air pollution pollutants in general. (Future global mortality from changes in air pollution attributable to climate change, Raquel A. Silva 2017 https://www.nature.com/articles/nclimate3354) (2014 above Impact on human health of climate changes Massimo Franchini) (Occurrence and persistence of future atmospheric stagnation events Daniel E. Horton https://www.nature.com/articles/nclimate2272)
The two main sources of air pollution's damaging effects on human health are ground level surface ozone and particulate matter. Surface ozone is produced as a chemical reaction from fossil fuel air pollutants catalyzed by solar warmth. Therefore surface ozone increases with global warming. It is highly irritant to the respiratory tract. The research is showing that surface warming and air circulation effects will increase the adverse effects from particulate matter.
“Ground level ozone is formed through photochemical reactions that involve nitrogen oxides (NOx), carbon monoxide (CO), methane (CH4), and volatile organic compounds (VOCs) in the presence of sunlight and elevated temperatures. Therefore as temperatures rise, many air pollution models project increased ozone production, especially within and surrounding urban areas. It is highly irritant to the entire respiratory tract. "There is observed evidence that tropospheric ozone increases in extreme heat, resulting in air pollution mortality” (IPCC 2014, 728-729).
There is evidence that global warming and climate change will increase the adverse impacts of air pollution pollutants in general. (Future global mortality from changes in air pollution attributable to climate change, Raquel A. Silva 2017 https://www.nature.com/articles/nclimate3354) (2014 above Impact on human health of climate changes Massimo Franchini) (Occurrence and persistence of future atmospheric stagnation events Daniel E. Horton https://www.nature.com/articles/nclimate2272)
2019 VIDEO Planetary Health: The Future is Now
WHO 2019 Top health threats are air pollution and climate change
8 March 2021 research
Keep warming under 1.5°C to stop tropics becoming too hot to live
8 May 2020. Many regions already affected
Keep warming under 1.5°C to stop tropics becoming too hot to live
8 May 2020. Many regions already affected

6 Sept 2021. Over 200 health journals call on world leaders to address 'catastrophic harm to health' from climate change
April 2021. Fossil fuel air pollution kills 10 million/year
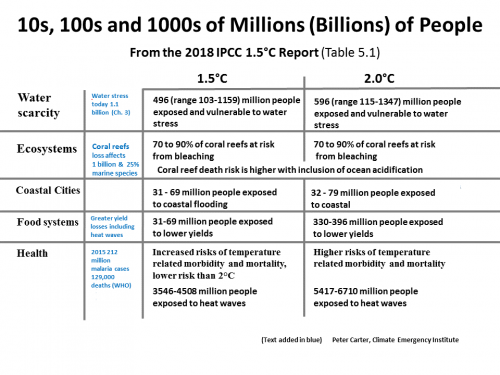
COMMITMENT Fundamental to the effects of global climate change on lives and health is the already climate system committed degree of climate change, which is much higher today's temperature increase. While the science protects impacts up to 2100, today's committed temperature increase (equilibrium warming) and impacts continues for many 100s of years after 2100.
Globally disastrous 1.5C is absolutely unavoidable (2030) and without immediate rapid emissions decline 2C is unavoidable by 2050. and at least 2C long-term equilibrium warming is committed (not including extra heating from feedbacks). Government policy commitment is 2.8C by 2100 (UNEP 2021)- higher after 2100
Globally disastrous 1.5C is absolutely unavoidable (2030) and without immediate rapid emissions decline 2C is unavoidable by 2050. and at least 2C long-term equilibrium warming is committed (not including extra heating from feedbacks). Government policy commitment is 2.8C by 2100 (UNEP 2021)- higher after 2100
May 2022 Inter-academy
Health in the Climate Emergency: A global perspective
Health in the Climate Emergency: A global perspective